Most traumatized adults are not conscious of the profound ways in which the past permeates their thoughts, emotions, decisions, and actions on a daily basis. Nor do their partners recognize the way the trauma of the significant other dictates their own lives.
Most traumatized adults are not conscious of the profound ways in which the past permeates their thoughts, emotions, decisions, and actions on a daily basis. Nor do their partners recognize the way the trauma of the significant other dictates their own lives.
It’s natural for all of us to see only that which is directly in front of us. We get caught up in the moment and fail to see the shadows of a past that lurks behind the present-day crisis. The demons battled by the trauma survivor are not in the partner’s line of vision. Even the trauma survivor may be in the dark as to the source of unwanted feelings and thoughts. The intrusive traumatic images, fear, and anger are like fireworks exploding in the survivor’s brain, while the explosions are completely invisible and inaudible to everyone else.
Like an animal cowering from the noisy celebrations on the Fourth of July, triggered individuals become withdrawn and quick-tempered, pushing others away in an attempt to find safety and comfort. Their significant others are often blind and deaf to what is happening on the inside of the person they love. They see only the inexplicable emotional wall. They feel shut out, lonely, and hurt, which may turn quickly into outrage. Trauma survivors are typically unable to respond with empathy to their partner’s underlying hurt, but react immediately and reflexively to their outrage. The anger they feel from their partner may be perceived as an assault, leading to escalating fear, pain, and loneliness—and so the chasm grows. The partner in turn may feel increasingly alienated, hurt, angry, and fearful.
Eventually, the partner comes to resemble the trauma survivor with whom he or she is struggling to relate–reactive, defensive, and searching for relief from emotional pain. In fact, the partner is suffering a vicarious traumatization. As the partner’s symptoms and reactions escalate, so do the symptoms of the trauma survivor. Both individuals can quickly become caught up in an endless negative feedback loop of reactivity. The physical closeness that used to trigger the release of love hormones may now triggers the release of stress hormones for them both. Increased closeness equals increased anxiety and stress.
Yet–it is possible for a “trauma couple” to heal. Neither partner started the relationship intending to cause hurt to the other. Seeking help from a professional is an important step, as an understanding third party can help sort out the stuck patterns and treat the traumas that lie at the root of everything. The professional can help the partners communicate from an understanding that neither is to blame and both are equally responsible for becoming part of the healing process. If just one partner takes the risk of letting go of defenses, it can be enough to interrupt the negative feedback loop and begin a new, healthier pattern of communication, with the help of a therapist. The alternative is a perpetual stand-off, like two cowboys standing in the dust with guns drawn and ready.
It requires courage for partners to explore their triggers and call themselves out on their own unhealthy methods of self-defense. It requires a willingness to be vulnerable to open up emotionally and share deeper feelings. It requires commitment to set aside fear and really listen to the other without blame or guilt. Both partners are likely to struggle and fall back into old patterns due to the underlying traumas and triggers, but if they can learn to give one another the benefit of the doubt and let go of trivial offenses, they will each come to see the real person behind the survival mechanisms of the other. If both partners practice staying emotionally present to one another, their mutual sense of understanding and compassion can grow and deepen into a strong and loving relationship.
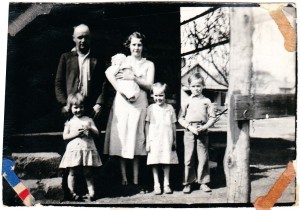
Photo Credit: Dollar Photo Club